Including students in course redesign pays dividends to the institution, the faculty involved, and the students themselves.

Traditional approaches to medical school education feature standard one-hour lectures, which has fostered a culture in which passive-learning environments promote low attendance, uneven quality and coordination between lecturers, and poor retention of content. To address these concerns, medical educators are increasingly turning to blended learning environments (that feature technology-enhanced learning solutions) and to educational strategies intended to promote active-learning. At the University of Miami Miller School of Medicine (UMMSM), between 2014 and 2019 we implemented learner-centered strategies in portions of our first- and second-year medical school curriculum.
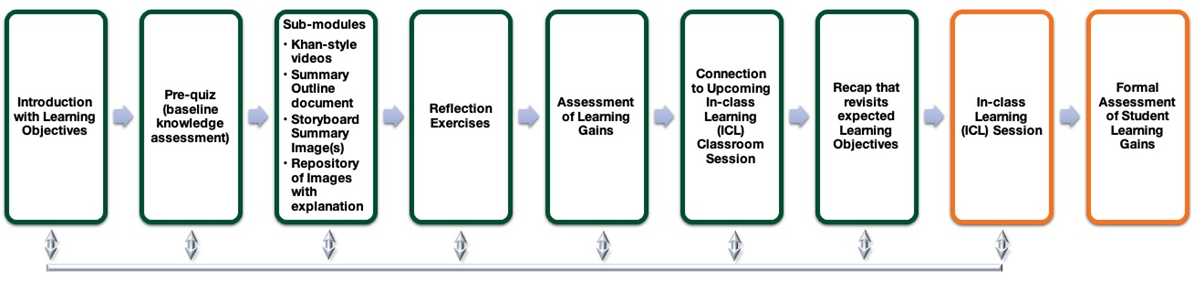
We developed a conceptual model that helps visualize how technology-enhanced learning was blended with face-to-face experiences (see figure 1). In the model, green boxes represent online activities and content (self-guided online learning modules), and orange boxes represent activities associated with face-to-face sessions (in-class learning sessions). Additionally, a faculty development infrastructure (with checklists, resources, and surveys) enhanced communication during our collaborative course design projects.Footnote1 This iterative course design process, which included consultations, content review, rapid prototyping, course preparation, and faculty coaching, involved collaboration across course coordinators, faculty members, and medical education staff members.
A central component of the faculty support team was the medical education student fellow, who served as a liaison between course coordinators and the educational technology team. Fellows were recruited annually via a national search and had already completed at least the first two years of medical school. Each fellow served for one full calendar year and received a stipend with travel funding. During their year at UMMSM, fellows became trusted members of the internal medical education community and regularly interacted with the academic deans. Fellows were mentored by an in-house educational expert, who oversaw the initiative and facilitated collaborations with medical education senior leadership and faculty members.
Interviews with Fellows
During a five-year retrospective evaluation of our initiative, we engaged in conversation with the five medical education student fellows who passionately served as our faculty liaisons. Specifically, we hoped to gain insight into their perspectives on the following items:
- How their experience as a fellow was aligned with national trends in medical education
- The degree to which they were able to transfer their experiences into professional growth
- Ways in which their experiences promoted educational, professional, and leadership growth
- Their satisfaction with the fellowship
A synthesis of their reflective contributions is featured in table 1.
Table 1. Synthesis of interview that aligns focal items with emergent themes and representative quotes
| Focus | Emergent Themes | Representative Quotation |
|---|---|---|
|
Alignment with National Trends |
Provided opportunities to actively participate in medical education reform efforts through their interactions with students, faculty, and medical education leadership at both local and national levels. |
"The medical education fellowship position helped me play an active role in rethinking how we approach teaching and learning in medical school." |
|
Transfer of Experiences |
Became trusted community members and medical education leaders, as evidenced by their participation in national conferences, accreditation committees, and curricular design teams. |
"My deepened understanding to the structure of undergraduate medical education allowed me to be a part of my university's LCME accreditation committee, and I was able to speak to some of the nuances of medical education with my peers to broaden their understanding of what occurs in the background." |
|
Growth and Development |
Enriched professional development by helping develop critical skillsets needed by emerging leaders in academic medicine, which includes the following: effective collaboration, teamwork, complex project management, curricular development, and the science of learning. |
"I significantly improved workplace task management and interpersonal skills. This has been useful now that I am a resident regularly navigating conflicting goals in an academic department." |
|
Satisfaction |
Productive time spent that helped develop valuable mentor–mentee relationships, promote reflection-on-practice, and foster a sense of gratitude for the unexpected experiences. |
"I do not think I would have matched into my residency were it not for my fellowship experience—it separated me from the rest of the applicants and showed that I was able to devote myself to a long-term project and accomplish something as a part of a team." |
Analysis of the fellows' responses yielded insight into how the fellowship program helped them mature professionally. For example, they conveyed how important this opportunity was in terms of developing their self-efficacy with taking active leadership roles in academic medicine. In fact, some translated that new confidence directly into service at their home institutions by participating in accreditation committees, assisting with curricular overhauls, and managing complex projects. These are fine characteristics on display from our future physicians and leaders in academic medicine!
Practical Considerations
Although this summary focused on an initiative within preclinical medical education, educators across all disciplines might benefit from partnering with students. A variety of opportunities (paid/unpaid, formal/informal) can potentially be generated that can form longitudinal experiences (see table 2). Alignment of faculty needs/objectives with fiscal limitations and logistical boundaries would determine appropriate student–faculty partnerships.
Keeping costs low is challenging for myriad reasons yet is critical in a pandemic ecosystem. One solution may be to create grassroots faculty support initiatives that can help foster innovation and creativity. Students-as-partners can become central figures within a network of educators, academic technologists, instructional designers, and content creators to support faculty needs. For example, they might generate course material and help with course redesigns. With formalized relationships, students-as-partners can support faculty members while gaining opportunities to master critical skills, such as effective communication, autonomy, and project management.
As our fellows revealed, both the faculty member and the student-partner are rewarded through their valuable mentor–mentee relationships. The result is far deeper than a transactional relationship. It extends the boundaries of the traditional teacher–learner experience and creates mechanisms for true collaboration and shared ownership of innovative contributions. Skillsets, passions, and areas of expertise are merged into a common focus of excellence and growth that help bypass organizational, fiscal, and logistical obstacles.
Table 2. Practical considerations to help educators implement student partnerships
| Level | Type of Student–Faculty Partnership | Examples |
|---|---|---|
|
Undergraduate |
Service Learning |
A team of students earned service-learning hours (required for graduation at their institution) to conduct usability tests of new interactive learning objects for a junior instructor. |
|
Internship |
An advanced student partnered with a faculty member to build a new course in the university's learning management system and added significant value by using graphic design skills to generate illustrations and visuals. |
|
|
Senior Thesis / Honors Project |
Student and faculty collaborated to conduct a literature search and meta-analysis that summarized advancements in blended learning course designs within their discipline. |
|
|
Graduate |
Teaching Assistants |
A paid teaching assistant partnered with a faculty member to help record and edit screengrab videos, which ultimately replaced lectures with a blended learning course redesign. |
|
Research Assistants |
A faculty member partnered with a graduate student (who received a stipend and tuition remission) to conduct education research and published an article that they co-authored. |
|
|
Fellowship |
Following a national search, a fellowship was provided to an individual who dedicated an academic year to curricular redesign support and scholarship of teaching and learning (SoTL). |
Summary
Many faculty members are saddled with research and service commitments that might limit their ability to innovate with curricular redesigns. However, using advanced-level students as partners in the course design/development process may help overcome these kinds of barriers. These collaborative relationships have the added value of establishing mentor–mentee relationships that benefit both parties. Although this conversation focused on a medical school initiative, we encourage critical stakeholders from other disciplines to consider adopting this collaborative approach to next-generation educational solutions in any educational context.
Related Resources
- David Green, "Using Action Maps to Sustain Technology-Enriched Academic Transformation Initiatives," EDUCAUSE Review, June 14, 2018.
- David P. Green, "Next-Generation Medical Education: Facilitating Student-Centered Learning Environments," ELI Brief, March 2016.
- David Green, "Teaching with Technology: Facilitating Blended Learning in Medical Education," ELI Webinar, March 28, 2016.
Acknowledgments
We gratefully acknowledge the following people and teams at the University of Miami for their leadership, vision, and friendship:
- Alex J. Mechaber, MD, FACP, former Senior Associate Dean for Undergraduate Medical Education at UMMSM, now the Associate Vice President for Physician Licensure Programs at the National Board of Medical Examiners (NBME)
- Mark O'Connell, MD, former Senior Associate Dean for Educational Development at UMMSM (retired)
- Barry Issenberg, MD, the Michael S. Gordon Professor of Medicine and Medical Education, Director of the Gordon Center for Research in Medical Education, and Senior Associate Dean for Research in Medical Education
- Allan Gyorke, Associate Vice President for IT, Assistant Provost for Educational Innovation, and Chief Academic Technology Officer
- Solomon Pikarsky, Director of IT for Medical Education
- Laurence Gardner, MD, MACP, Executive Dean for Education and Policy
- The Learning Innovation and Faculty Engagement team at the University of Miami
- The Division for Innovations in Medical Education within the Educational Development Office at the University of Miami Miller School of Medicine
- Rishi Desai, MD, MPH, former Lead at Khan Academy Medicine, now the Chief Medical Officer at Osmosis
Note
- For more information about this effort, see David P. Green, "Next-Generation Medical Education: Facilitating Student-Centered Learning Environments," ELI Brief, March 2016. Jump back to footnote 1 in the text.
David Green was the Director of Educational Technologies within the University of Miami Miller School of Medicine's Educational Development Office, where he oversaw the Division for Innovations in Medical Education.
David Faber was a Medical Education Fellow with the University of Miami Miller School of Medicine's Educational Development Office (2014–15).
Preetha Kamath was a Medical Education Fellow with the University of Miami Miller School of Medicine's Educational Development Office (2017–18).
Matthew Kofoed was a Medical Education Fellow with the University of Miami Miller School of Medicine's Educational Development Office (2015–16).
Sean Schooley is was a Medical Education Fellow with the University of Miami Miller School of Medicine's Educational Development Office (2018–19).
Jared Senvisky was a Medical Education Fellow with the University of Miami Miller School of Medicine's Educational Development Office (2016–17).
© 2021 David Green, David Faber, Preetha Kamath, Matthew Kofoed, Sean Schooley, and Jared Senvisky. The text of this work is licensed under a Creative Commons BY-NC-ND 4.0 International License.
